Pelvic Organ Prolapse (POP) in Pelvic Floor Muscle Dysfunction: Protocol
1. Overview of Condition:
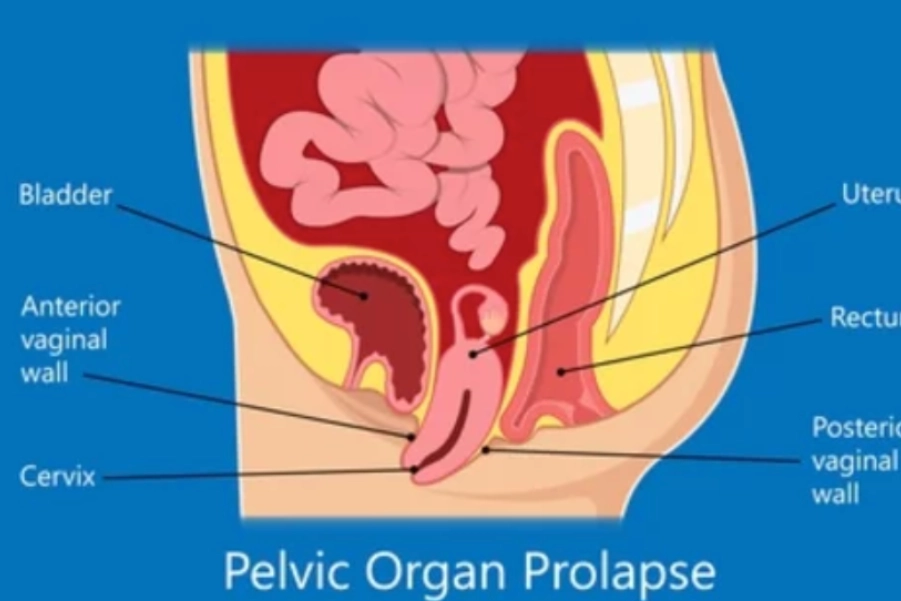
Pelvic Organ Prolapse (POP) is the descent or bulging of pelvic organs (bladder, uterus, rectum, or small intestine) into the vaginal canal due to weakened pelvic floor muscles and connective tissues. It commonly occurs in women post-childbirth, during menopause, or with aging, but can also be exacerbated by factors such as heavy lifting, chronic constipation, or obesity. POP manifests with symptoms like pelvic pressure, urinary incontinence, difficulty voiding, and bowel dysfunction.
Symptoms:
- Sensation of pelvic pressure, heaviness, or fullness.
- Vaginal bulging or visible prolapse of pelvic organs.
- Difficulty with bladder or bowel emptying (urinary retention, constipation).
- Urinary incontinence or frequent urination.
- Lower back or pelvic pain, and discomfort during intercourse.
Probable Deficits:
- Pelvic Floor Muscle Weakness: Reduced muscle tone and strength, insufficient support for pelvic organs.
- Connective Tissue Weakness: Damage to ligaments and connective tissues supporting pelvic organs.
- Bladder Dysfunction: Difficulty voiding the bladder due to pelvic floor dysfunction or prolapse.
- Bowel Dysfunction: Difficulty with bowel evacuation due to reduced pelvic floor support.
2. Assessment and Evaluation of Impairment:
A comprehensive clinical evaluation is necessary to assess the severity of POP, pelvic floor muscle function, and any associated bladder or bowel dysfunction.
Clinical Tools for Assessment:
- Patient History: Document childbirth history, surgical procedures (e.g., hysterectomy), chronic conditions (e.g., constipation), and lifestyle factors (e.g., obesity, heavy lifting).
- Pelvic Organ Prolapse Quantification (POP-Q): Standard tool to assess the degree of prolapse in relation to the vaginal walls.
- Pelvic Floor Muscle Assessment:
- Manual Muscle Testing (MMT): To evaluate muscle strength, tone, and endurance.
- Perineometer or EMG Biofeedback: For muscle strength evaluation and real-time feedback.
- Bladder Function Assessment:
- Bladder Diary: Track fluid intake, voiding patterns, and incontinence episodes.
- Post-Void Residual (PVR) Measurement: Assesses incomplete bladder emptying.
- Bowel Function Assessment: Investigate bowel movements, straining, and symptoms like fecal incontinence or incomplete evacuation.
3. Goal Setting:
The treatment aims to alleviate symptoms, improve pelvic floor muscle function, and prevent prolapse progression. The secondary goal is to optimize bladder and bowel function, enhance quality of life, and delay invasive procedures like surgery.
Specific Goals:
- Primary: Reduce pelvic pressure and heaviness, manage prolapse symptoms (e.g., bulging, incontinence), and prevent further prolapse.
- Secondary:
- Improve pelvic floor muscle strength and endurance.
- Enhance bladder and bowel function (voiding and evacuation).
- Increase awareness and self-management strategies for pelvic health.
- Improve sexual function and comfort.
- Prevent or delay the need for surgical intervention.
4. Recommended Interventions:
Electrotherapy:
- Pelvic Floor Electrical Stimulation (PFES): Enhances muscle strength, endurance, and coordination.
- Protocol: 10-20 minute sessions, 2-3 times weekly with low-frequency stimulation.
- Evidence: Lee et al. (2022) demonstrated PFES improves pelvic floor function and reduces prolapse symptoms.
Biofeedback Therapy:
- EMG Biofeedback: Helps patients learn pelvic floor activation and relaxation.
- Protocol: 10-15 minute sessions, 2-3 times weekly, progressing based on patient response.
- Evidence: Studies (Bo et al., 2023) support biofeedback for improving pelvic floor strength.
Pelvic Floor Muscle Training (PFMT):
- Strengthening and Coordination Exercises: Target both muscle strength and coordination to enhance pelvic organ support.
- Protocol:
- Strengthening: 3 sets of 10-15 contractions daily, with short and long hold techniques.
- Coordination: Incorporate relaxation and contraction exercises.
- Evidence: Neels et al. (2024) show PFMT improves pelvic floor strength and alleviates prolapse symptoms.
- Protocol:
Bladder and Bowel Training:
- Bladder Training: Timed voiding to optimize bladder function and alleviate urinary symptoms.
- Protocol: Gradually increase voiding intervals and encourage complete bladder emptying.
- Evidence: Fitzgerald et al. (2023) confirm bladder training improves control and reduces POP symptoms.
- Bowel Training: Improve bowel function through timed movements, high-fiber diet, and postural techniques.
- Protocol: Daily bowel training with focus on pelvic floor relaxation during defecation.
- Evidence: Wyman et al. (2022) highlight the importance of pelvic floor relaxation for managing constipation.
Lifestyle Modifications:
- Weight Management: Encourage weight reduction to relieve excess pressure on the pelvic floor.
- Protocol: Guidance on a balanced diet and physical activity for maintaining a healthy BMI.
- Evidence: Schultz et al. (2023) identify excess weight as a major risk factor for prolapse progression.
Pessaries:
- Pessary Use: For moderate to severe prolapse symptoms, a pessary provides mechanical support to pelvic organs.
- Protocol: Regular follow-up to assess fit, comfort, and potential complications.
- Evidence: Bo et al. (2023) showed pessaries are effective in relieving prolapse symptoms.
5. Precautions and Special Considerations:
- Chronic Constipation: Manage constipation effectively as it can worsen prolapse symptoms.
- Pregnancy/Postpartum: Be cautious postpartum, especially following recent deliveries; avoid overloading the pelvic floor during the recovery phase.
- Surgical History: Consider prior pelvic surgeries (e.g., hysterectomy), as these may affect rehabilitation strategies.
6. Reassessment, Criteria for Progression/Change in Care Plan:
Symptom Tracking:
- Use questionnaires (e.g., PFDI) to assess pelvic pressure and functional impact.
- Track bladder and bowel symptoms through diaries.
Functional Assessments:
- Monitor pelvic floor muscle strength with MMT or biofeedback.
- Reassess prolapse severity using the POP-Q system every 3-6 months.
Criteria for Progression:
- Reduction in pelvic pressure and heaviness.
- Improvement in pelvic floor strength and endurance.
- Enhanced bladder and bowel function.
- Symptom relief with pessary use or avoidance of surgery.
Disclaimer and Note:
This treatment protocol provides a framework for managing pelvic organ prolapse and related symptoms. However, treatment options should be chosen based on individual assessment and appropriateness. Consultation with a qualified healthcare provider is essential for personalized care. The content is for informational purposes only and should not replace professional medical advice or treatment.
References:
- Lee, J. Y., et al. (2022). Effectiveness of Pelvic Floor Electrical Stimulation in Pelvic Organ Prolapse Treatment. Urology Journal.
- Bo, K., et al. (2023). Biofeedback Therapy in Pelvic Floor Rehabilitation for Pelvic Organ Prolapse. Journal of Urogynecology.
- Neels, H., et al. (2024). Pelvic Floor Muscle Training for Pelvic Organ Prolapse: A Meta-analysis. International Journal of Women’s Health.
- Fitzgerald, M. P., et al. (2023). Bladder Training in Women with Pelvic Organ Prolapse: A Clinical Approach. Neurourology and Urodynamics.
- Schultz, M., et al. (2023). Pelvic Floor Rehabilitation and Lifestyle Modifications in Pelvic Organ Prolapse. Journal of Women’s Health Physiotherapy.