Neurological Physiotherapy Treatment Protocol for Posterior Cerebral Artery Stroke Survivor
Overview of Conditions
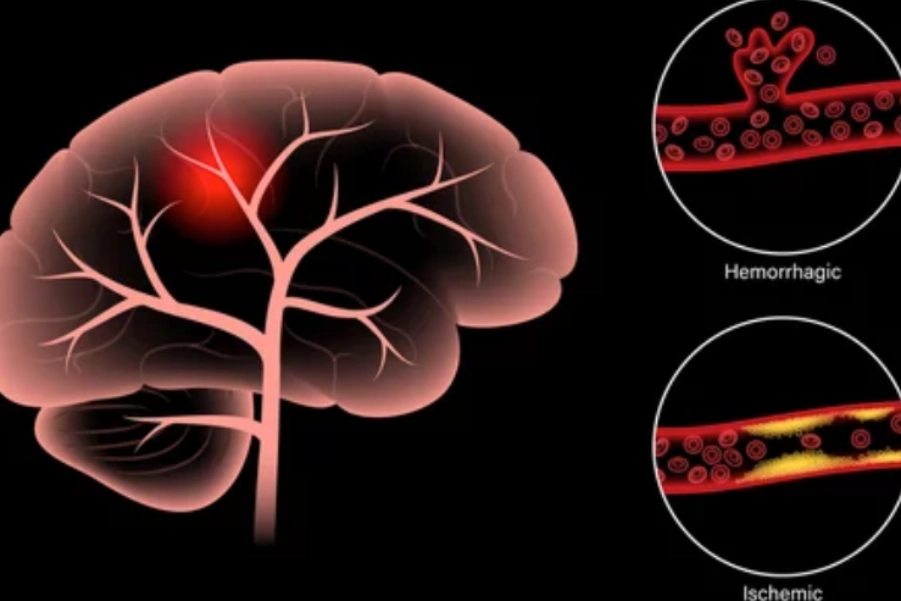
A Posterior Cerebral Artery (PCA) stroke occurs when there is ischemia or infarction in the posterior cerebral artery, which provides blood to the occipital lobe, thalamus, and parts of the parietal lobe. This type of stroke can lead to deficits in vision, sensory processing, and spatial awareness, and may also affect higher cognitive functions like memory and executive functions due to involvement of the thalamus and occipital cortex.
Common Clinical Manifestations of PCA Stroke:
- Visual Impairments: Most commonly, homonymous hemianopia (loss of vision in the same half of the visual field in both eyes).
- Sensory Deficits: Impaired sensation, especially proprioception, on the contralateral side of the body.
- Cognitive Deficits: Memory impairments, particularly spatial memory, and disruptions in executive functions.
- Motor Impairments: Hemiparesis or hemiplegia, especially affecting fine motor tasks.
- Gait and Balance Dysfunction: Challenges in balance, particularly in environments with obstacles or poor lighting.
Symptomatology and Probable Deficits
- Visual Deficits:
- Homonymous hemianopia, which complicates object recognition and navigation.
- Visual neglect or inattention to the affected side.
- Sensory Deficits:
- Contralateral sensory loss, particularly in proprioception, causing difficulties in balance and spatial orientation.
- Motor Deficits:
- Hemiparesis or hemiplegia affecting both upper and lower limbs.
- Fine motor difficulties, hindering functional tasks like buttoning clothes or writing.
- Cognitive Deficits:
- Difficulty with memory, particularly spatial and object recognition.
- Executive dysfunction, including planning and problem-solving challenges.
- Gait and Balance Dysfunction:
- Difficulty maintaining balance, especially in challenging environments (e.g., obstacles or poor lighting).
- Coordination issues that affect safe and efficient movement.
Assessment and Evaluation
- Functional Task Impairment Assessment:
- Fugl-Meyer Assessment of Motor Recovery (FMA): Assesses motor recovery in the upper and lower limbs.
- Berg Balance Scale (BBS): Evaluates balance and fall risk.
- 10-Meter Walk Test (10MWT): Assesses walking speed and functional mobility.
- Montreal Cognitive Assessment (MoCA): Evaluates cognitive functions, including memory, attention, and executive function.
- Visual Field Tests: To assess homonymous hemianopia and other visual impairments.
- Key Functional Impairments:
- Visual Impairment: Difficulty detecting or avoiding obstacles, particularly on the affected side.
- Motor Dysfunction: Hemiparesis, particularly with fine motor tasks.
- Sensory Deficits: Reduced proprioception affecting balance and gait.
- Cognitive and Memory Impairment: Difficulty recalling locations, tasks, or objects, impacting daily life and mobility.
Goal Setting
- Short-term Goals (2-4 weeks):
- Improve motor function, particularly fine motor control.
- Address visual deficits using compensatory strategies.
- Improve balance and reduce fall risk.
- Long-term Goals (6-12 weeks):
- Achieve independent mobility with improved gait and balance.
- Enhance cognitive functions, including memory, problem-solving, and spatial awareness.
- Enhance performance in activities of daily living (ADLs).
Recommended Interventions
- Vision Rehabilitation and Compensatory Strategies
- Description: Focused training and adaptive strategies for visual deficits, including homonymous hemianopia.
- Scientific Basis: Vision rehabilitation techniques, including scanning training and use of compensatory devices, can significantly improve mobility and safety (Baker et al., 2020).
- Protocol:
- Train scanning strategies to compensate for visual field loss.
- Use devices like prism glasses to assist with visual navigation.
- Implement functional tasks to reinforce scanning and situational awareness (e.g., reading, locating objects).
- Sensory Re-education and Proprioceptive Training
- Description: Exercises to improve sensory awareness and proprioception.
- Scientific Basis: Proprioceptive training has been shown to enhance sensory discrimination and motor function, crucial for balance and motor coordination (Mackenzie et al., 2022).
- Protocol:
- Use tactile and proprioceptive feedback tasks (e.g., object identification through touch).
- Incorporate balance and weight-shifting exercises.
- Utilize proprioceptive neuromuscular facilitation (PNF) techniques to enhance motor coordination.
- Motor Relearning Program (MRP)
- Description: A structured program focusing on retraining motor patterns through repetitive practice.
- Scientific Basis: MRP enhances neuroplasticity by strengthening neural pathways and promoting muscle recruitment (Ada et al., 2021).
- Protocol:
- Begin with simple, controlled movements (e.g., reaching, grasping).
- Progress to complex tasks such as walking or performing ADLs.
- Provide feedback and guide the patient through the motor learning process.
- Gait Training and Balance Rehabilitation
- Description: Targeted exercises to enhance gait and balance, emphasizing visual and proprioceptive feedback.
- Scientific Basis: Gait and balance training enhances postural control and walking efficiency by promoting neural adaptation (Hornby et al., 2020).
- Protocol:
- Begin with supported walking and progress to unassisted walking.
- Include tasks like obstacle avoidance, turning, and walking on varied surfaces.
- Incorporate visual feedback exercises to improve spatial awareness.
- Cognitive and Memory Rehabilitation
- Description: Cognitive tasks to enhance memory, attention, and executive functions.
- Scientific Basis: Cognitive rehabilitation can improve memory and executive function, particularly in individuals affected by thalamic or occipital damage (Cicerone et al., 2021).
- Protocol:
- Engage in memory exercises focusing on spatial and visual tasks.
- Use apps and games targeting cognitive skills such as attention and problem-solving.
- Encourage attention-improving strategies like reducing distractions.
Precautions and Special Considerations
- Visual Impairments: Ensure a well-lit, clutter-free environment to minimize fall risk due to visual field deficits.
- Motor Dysfunction: Start with low-intensity tasks and gradually progress as strength and motor control improve.
- Cognitive and Memory Deficits: Provide clear instructions, use visual aids, and incorporate breaks to manage cognitive fatigue.
Reassessment
Reassess the patient every 2-4 weeks using functional outcome measures such as the FMA, BBS, 10MWT, and MoCA. Adjust the treatment plan based on improvements in motor function and cognitive abilities.
Disclaimer:
This treatment protocol provides general guidelines for the rehabilitation of patients with PCA stroke. It is essential that treatment options be selected appropriately based on the individual patient’s condition, abilities, and response to therapy. Consultation with a qualified healthcare provider is advised for personalized care and treatment plans.
References:
- Baker, A. L., et al. (2020). “Vision rehabilitation techniques in patients with homonymous hemianopia after stroke: A systematic review.” Journal of Stroke and Cerebrovascular Diseases, 29(3), 104529.
- Mackenzie, G., et al. (2022). “Proprioceptive training for stroke rehabilitation: Evidence from systematic reviews.” Neurorehabilitation and Neural Repair, 36(2), 89-99.
- Ada, L., et al. (2021). “Motor relearning program for stroke survivors: A systematic review and meta-analysis.” Clinical Rehabilitation, 35(7), 1159-1171.
- Hornby, T. G., et al. (2020). “Effects of gait training on post-stroke gait: A systematic review and meta-analysis.” Stroke, 51(3), 623-633.
- Cicerone, K. D., et al. (2021). “Cognitive rehabilitation interventions for stroke survivors: A review of current research.” Neuropsychological Rehabilitation, 31(4), 676-697.