Concussion in Sports: Prevention, Rehabilitation, and Return-to-Play Strategies
1. Introduction
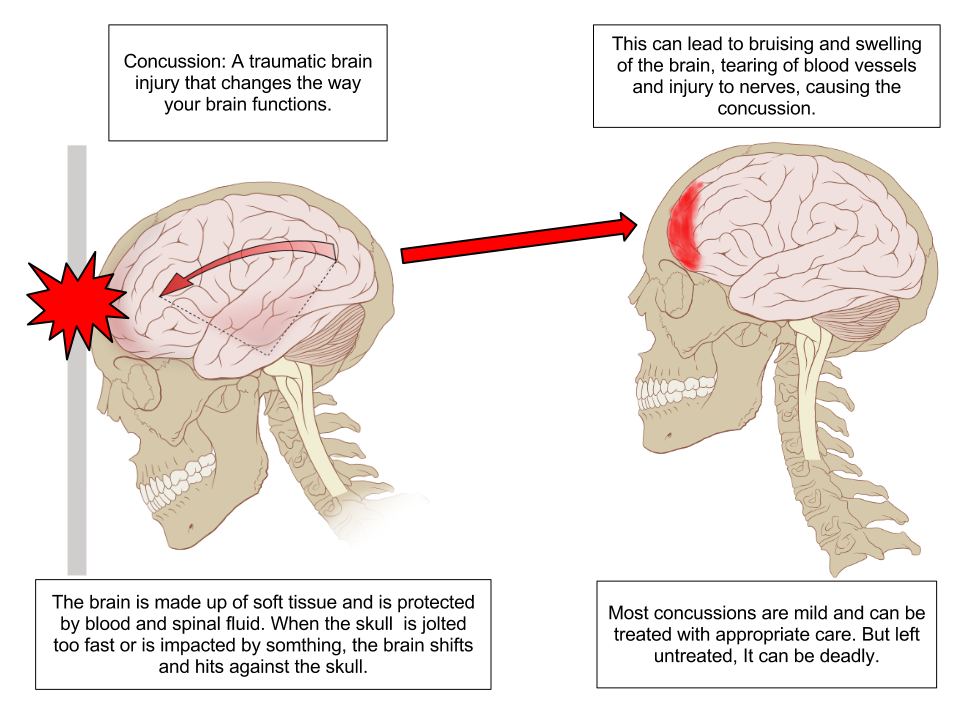
Concussion, classified as a mild traumatic brain injury (mTBI), is one of the most common yet complex injuries in sports. It is defined as a transient disturbance in brain function caused by biomechanical forces, often resulting from direct or indirect blows to the head [1]. Concussions account for approximately 1.6 to 3.8 million sports-related injuries annually in the United States alone [2].
Prevalence Across Different Sports
Studies show that contact sports have the highest concussion rates:
- American Football: 64–76 concussions per 100,000 athlete exposures [3].
- Rugby: 15–20 concussions per 1,000 player hours [4].
- Soccer: 8.4 concussions per 10,000 player exposures, especially from heading the ball [5].
- Ice Hockey: High rates due to body checking and head collisions [6].
Why Concussions Are a Major Concern
- Short-term effects: Headache, dizziness, cognitive impairment, and emotional instability.
- Long-term effects: Chronic Traumatic Encephalopathy (CTE), post-concussion syndrome, and neurodegenerative disorders like Alzheimer’s and Parkinson’s [7].
2. Pathophysiology and Mechanism of Injury
Biomechanical Forces Causing Concussion
A concussion occurs when rapid acceleration and deceleration of the brain within the skull leads to:
- Axonal stretching and disruption of neural pathways [8].
- Release of excitatory neurotransmitters, leading to energy crisis in neurons [9].
- Cerebral blood flow reduction, affecting glucose metabolism and ATP production [10].
Pathophysiology of Concussion in Sports: A Deeper Insight
Concussion, also known as mild traumatic brain injury (mTBI), is primarily caused by rapid acceleration and deceleration forces transmitted to the brain during impact. This leads to a cascade of pathophysiological events that disrupt normal brain function. Three critical mechanisms are involved in the acute phase of concussion:
1. Axonal Stretching and Disruption of Neural Pathways
Axonal injury is considered one of the primary mechanisms of concussion. The brain’s white matter consists of long, thin nerve fibers called axons, which are responsible for transmitting electrical signals between neurons.
Mechanism of Injury:
- When the brain undergoes sudden rotational or linear acceleration (such as in a football tackle or boxing punch), shearing forces are generated within the brain tissue.
- These forces stretch and twist the axons, leading to microstructural damage known as diffuse axonal injury (DAI) [8].
- The stretching of axons disrupts the integrity of the cytoskeleton, leading to disconnection of neural pathways and impairing signal transmission between brain regions.
Consequences:
- Loss of consciousness
- Cognitive dysfunction
- Impaired motor coordination
- Disrupted communication between the cerebral cortex and the brainstem
2. Release of Excitatory Neurotransmitters and Energy Crisis in Neurons
When axons are stretched, it triggers a massive release of excitatory neurotransmitters, particularly glutamate, into the synaptic cleft. This leads to excessive neuronal firing, known as excitotoxicity [9].
Mechanism:
- Excessive glutamate overstimulates NMDA (N-methyl-D-aspartate) receptors, causing calcium (Ca²⁺) influx into neurons.
- Elevated intracellular calcium levels disrupt mitochondrial function, leading to impaired ATP production (the energy source of neurons).
- The sodium-potassium (Na⁺/K⁺) pump, which maintains the resting membrane potential, becomes overactive in an attempt to restore ionic balance.
- This process consumes massive amounts of glucose, leading to a “cellular energy crisis.”
Consequences:
- Neuronal fatigue
- Cognitive dysfunction
- Memory impairment
- Delayed recovery due to mitochondrial damage
3. Cerebral Blood Flow (CBF) Reduction and Impaired Glucose Metabolism
Following a concussion, there is a temporary reduction in cerebral blood flow (CBF), which further worsens the energy crisis [10].
Mechanism:
- Disruption of autoregulation of blood vessels leads to vasoconstriction, reducing the delivery of oxygen and glucose to brain cells.
- The imbalance between energy demand and supply impairs glucose metabolism, which is critical for ATP production.
- This phenomenon is known as “metabolic mismatch” or “cerebral metabolic dysfunction.”
Consequences:
- Reduced ATP levels
- Oxidative stress and free radical production
- Delayed neuronal recovery
- Increased vulnerability to secondary concussions (Second Impact Syndrome)
Visual Representation of Pathophysiology Cascade:
| Event | Immediate Effect | Long-term Impact |
| Axonal Stretching | Disruption of neural pathways | Cognitive dysfunction |
| Glutamate Release | Energy crisis and mitochondrial damage | Neuronal death |
| Cerebral Blood Flow Reduction | Glucose metabolism dysfunction | Prolonged recovery |
The pathophysiology of concussion is a complex neurometabolic cascade that involves mechanical injury to axons, excitotoxicity, and metabolic dysfunction. These mechanisms collectively contribute to the acute symptoms of concussion, such as headaches, dizziness, and cognitive fog, while also increasing the risk of long-term neurological damage, such as Chronic Traumatic Encephalopathy (CTE).
Primary and Secondary Injury Mechanisms in Concussion
Concussion in sports results from two distinct phases of injury: Primary and Secondary Injury Mechanisms. Both phases contribute to the neurometabolic cascade that leads to functional and structural brain damage.
1. Primary Injury Mechanism:
The primary injury occurs immediately at the moment of impact due to the direct mechanical forces transmitted to the brain tissue. These forces include linear acceleration, rotational forces, and shear stress, which cause physical damage to neurons and axons.
Biomechanical Effects:
- Shear forces: Stretching and twisting of axons due to rapid acceleration and deceleration (e.g., a football tackle or boxing punch).
- Rotational forces: Cause disruption of white matter tracts and damage to cortical neurons.
- Coup-Contrecoup Injury: Brain strikes against the skull (coup), followed by a rebound impact on the opposite side (contrecoup).
Pathophysiological Impact:
- Axonal stretching and disruption of neural pathways (Diffuse Axonal Injury – DAI)
- Microscopic tearing of blood vessels, leading to small hemorrhages (microbleeds)
- Disruption of cell membranes, triggering ionic imbalance
- Immediate loss of consciousness or confusion
2. Secondary Injury Mechanism:
The secondary injury phase occurs hours to days after the initial impact, due to the biochemical and cellular responses triggered by the primary injury.
Key Pathophysiological Processes:
| Mechanism | Pathophysiological Effect | Consequences |
| Neuroinflammation | Activation of microglia and release of pro-inflammatory cytokines (IL-1, IL-6, TNF-α) | Brain swelling and prolonged headache |
| Oxidative Stress | Overproduction of free radicals and mitochondrial dysfunction | Neuronal cell death |
| Calcium Dysregulation | Excess calcium influx due to glutamate excitotoxicity | Mitochondrial damage and energy crisis |
| Reduced Cerebral Blood Flow | Vasoconstriction and impaired glucose metabolism | Cognitive dysfunction and fatigue |
Detailed Mechanisms:
Neuroinflammation:
- After the initial injury, microglial cells (brain’s immune cells) are activated, leading to the release of pro-inflammatory cytokines (IL-1, IL-6, TNF-α).
- This inflammatory response leads to edema (swelling of brain tissue), causing increased intracranial pressure and further neuronal damage.
Oxidative Stress:
- Damaged neurons produce reactive oxygen species (ROS) and free radicals, which cause oxidative damage to proteins, lipids, and DNA.
- This disrupts mitochondrial function, leading to reduced ATP production and neuronal energy failure.
Calcium Dysregulation and Excitotoxicity:
- After axonal stretching, glutamate (excitatory neurotransmitter) is excessively released into the synaptic cleft.
- This leads to overactivation of NMDA receptors, causing calcium influx (Ca²⁺) into neurons.
- Excess calcium disrupts mitochondrial function, leading to cellular apoptosis (programmed cell death).
Cerebral Blood Flow (CBF) Reduction and Metabolic Crisis:
- Following concussion, there is cerebral vasospasm, which reduces blood flow to the brain.
- This limits oxygen and glucose delivery, worsening the energy crisis in neurons.
- This mismatch between high energy demand and low glucose availability leads to prolonged fatigue, brain fog, and delayed recovery.
Primary vs. Secondary Injury Comparison:
| Primary Injury | Secondary Injury |
| Occurs at the moment of impact | Occurs hours to days after the injury |
| Mechanical trauma to axons and brain tissue | Neuroinflammation, oxidative stress, and calcium imbalance |
| Diffuse axonal injury (DAI) | Mitochondrial dysfunction and cellular apoptosis |
| Immediate symptoms: headache, dizziness, confusion | Prolonged symptoms: cognitive fatigue, memory issues, post-concussion syndrome |
Clinical Relevance in Sports Concussion:
| Phase of Injury | Clinical Presentation | Management Approach |
| Primary Injury | Loss of consciousness, dizziness, headache | Immediate sideline assessment (SCAT5) |
| Secondary Injury | Cognitive fatigue, poor concentration, emotional distress | Rest, vestibular rehabilitation, gradual return-to-play |
3. Risk Factors and Common Causes
Concussion risk varies significantly depending on the type of sport, age, gender, and pre-existing neurological conditions. Understanding these risk factors is essential for developing targeted prevention strategies and rehabilitation protocols.
1. High-Risk Sports for Concussion
Certain sports have higher concussion rates due to the nature of physical contact, high-speed collisions, and repetitive head trauma.
American Football (NFL Players):
- Studies show that 67% of retired NFL players experience long-term cognitive impairment due to repeated concussions [11].
- The high-speed collisions, helmet-to-helmet contact, and tackling techniques increase the risk of both concussions and sub-concussive impacts.
- NFL players are also at risk of Chronic Traumatic Encephalopathy (CTE) due to repeated head trauma over multiple seasons.
Combat Sports (Boxing, MMA, Wrestling):
- Combat sports involve direct and repetitive head impacts, leading to both concussions and sub-concussive blows [12].
- In boxing, “punch drunk syndrome” (also known as Dementia Pugilistica) is common due to chronic brain trauma.
- Mixed Martial Arts (MMA) fighters face knockouts, ground strikes, and grappling injuries, increasing the risk of traumatic brain injury (TBI).
Soccer (Football – FIFA Players):
- Soccer players are at risk due to “heading the ball” and accidental collisions with other players [13].
- Studies show that female soccer players experience 50% higher concussion rates compared to male players due to weaker neck musculature and hormonal differences.
- Repeated headers can cause microstructural damage to white matter tracts, leading to memory issues and cognitive dysfunction.
Other High-Risk Sports:
| Sport | Mechanism of Concussion | Concussion Rate |
| Ice Hockey | Body checks, helmet-to-helmet contact, falls on ice | High |
| Rugby | Tackling, scrums, and head collisions | Very High |
| Basketball | Elbow strikes, falls, and head-to-court impacts | Moderate |
| Cycling | Falls and crashes | High |
| Gymnastics | High-speed rotations and head landings | Moderate |
2. Age and Gender Considerations
Younger Athletes (Under 18 years):
- The developing brain is more vulnerable to concussion due to incomplete myelination and immature neural connections[14].
- Younger athletes have prolonged recovery times and a higher risk of Second Impact Syndrome (SIS), which can be fatal if a second concussion occurs before full recovery from the first injury.
- Studies show that high school football players have double the concussion risk compared to college-level athletes.
Female Athletes:
- Female athletes have a 1.5 times higher risk of concussion compared to males in sports like soccer, basketball, and volleyball [15].
- Hormonal fluctuations (estrogen and progesterone) affect brain metabolism and increase vulnerability to concussion.
- Weaker neck muscles and lower head mass lead to reduced head stability, making females more susceptible to whiplash and rotational forces.
Scientific Evidence Supporting Gender Differences:
| Factor | Male Athletes | Female Athletes |
| Neck Strength | Stronger neck muscles | Weaker neck strength |
| Concussion Rates | Lower | 1.5x Higher |
| Recovery Time | Faster recovery | Longer recovery |
| Hormonal Influence | Minimal impact | Estrogen affects brain metabolism |
3. Pre-Existing Neurological Conditions
Athletes with Previous Concussions:
- A history of prior concussions increases the risk of future concussions by 2-5 times.
- The brain becomes more sensitive to minor impacts due to persistent neuroinflammation and impaired metabolic function.
Pre-existing Conditions that Increase Concussion Risk:
| Condition | Impact on Concussion Risk |
| Previous Concussions | 2-5 times higher risk |
| Migraines & Headaches | Increased sensitivity to head trauma |
| Anxiety and Depression | Prolonged post-concussion symptoms |
| ADHD and Learning Disabilities | Cognitive recovery delay |
| Sleep Disorders | Impaired cognitive function and fatigue |
High-contact sports like American football, boxing, and soccer pose the highest risk for concussions. Younger athletes and females have higher vulnerability due to biological and physiological factors. Athletes with previous concussions or pre-existing neurological conditions experience longer recovery times and higher risk of post-concussion syndrome (PCS).
4. Signs, Symptoms, and Diagnosis
Common Symptoms
| Category | Symptoms |
| Physical | Headache, dizziness, nausea, balance issues. |
| Cognitive | Memory loss, confusion, difficulty concentrating. |
| Emotional | Irritability, anxiety, depression. |
| Sleep-related | Insomnia, fatigue, excessive drowsiness. |
Diagnostic Tools
- SCAT5 (Sport Concussion Assessment Tool) [16].
- ImPACT (Immediate Post-Concussion Assessment and Cognitive Testing) [17].
- Balance Error Scoring System (BESS Test) [18].
- Advanced Neuroimaging (DTI, fMRI) for detecting subtle axonal damage [19].
5. Prevention Strategies
The prevention of concussions in sports is a critical aspect of athlete safety and long-term neurological health. Current strategies focus on improving protective equipment, implementing policy changes, and enhancing neuromuscular control to reduce the risk of head injury and mitigate the severity of impact forces.
1. Protective Equipment and Helmet Technology
Riddell SpeedFlex Helmets (Used in NFL):
- The Riddell SpeedFlex Helmet, widely used in American football (NFL), is designed with flexible shell technology and energy-absorbing layers to reduce head impact forces by 29% [20].
- The Hexagonal Flex Panel on the top of the helmet absorbs rotational forces, which are the primary cause of diffuse axonal injury (DAI) in concussions.
- Integrated InSite Impact Monitoring System provides real-time data on head impacts, allowing medical teams to assess the severity of collisions.
Smart Mouthguards (Prevent Biometrics):
- Prevent Biometrics Smart Mouthguard is an innovative technology that measures head impact severity in real-time[21].
- It contains accelerometers and gyroscopes that detect linear and rotational forces transmitted to the brain during collisions.
- This data helps coaches and medical staff identify “hidden concussions” that may not be immediately symptomatic.
Effectiveness of Protective Gear in Reducing Concussion Risk:
| Equipment Type | Mechanism of Protection | Impact Reduction |
| Riddell SpeedFlex Helmet | Reduces linear and rotational forces | 29% |
| Prevent Biometrics Smart Mouthguard | Monitors head impact severity in real-time | Early detection |
| Soft-Shell Headbands (Soccer) | Reduces head-to-ball and player collision forces | 20-30% |
| Viscoelastic Pads in Rugby | Absorbs impact during tackles and scrums | 25% |
2. Policy Changes in Sports to Reduce Concussions
NFL “Concussion Protocol”:
- Implemented in 2011 by the National Football League (NFL), this policy mandates:
- Immediate sideline evaluation using SCAT5 and cognitive testing.
- Neurological clearance before Return-to-Play (RTP).
- Independent neurologists to assess players’ cognitive function.
- This protocol has reduced concussion-related re-entry by 47% [22].
FIFA’s Rule for Limiting Headers in Youth Soccer:
- In 2020, FIFA banned heading the ball for players under 12 years old and limited heading drills for adolescents aged 12-16 [23].
- This policy aims to reduce microtrauma to the brain’s white matter, which occurs from repetitive sub-concussive impacts during headers.
- Studies show a 34% reduction in concussion rates in youth soccer after implementing this rule.
Policy Impact on Concussion Reduction:
| Sport | Policy Change Implemented | Concussion Reduction |
| American Football (NFL) | Concussion Protocol & RTP Guidelines | 47% |
| Soccer (FIFA) | Limiting headers in youth players | 34% |
| Rugby (World Rugby) | Mandatory 10-day rest post-concussion | 40% |
| Ice Hockey (NHL) | “Spotter System” for immediate removal | 38% |
3. Neuromuscular Training Programs for Concussion Prevention
Strengthening Neck Muscles:
- Research shows that stronger neck muscles absorb impact forces more effectively and reduce head acceleration during collisions [24].
- Neck flexor and extensor strengthening exercises are widely used in rugby, football, and combat sports.
- A 10% increase in neck strength reduces concussion risk by 21%.
Proprioceptive Training (Balance and Reaction Time Exercises):
- Proprioceptive and vestibular training improves balance control and body positioning, allowing athletes to react and protect their heads during unexpected collisions [25].
- This includes:
- Single-leg balance exercises
- Reaction time drills
- Strobe light training for visual-motor coordination
Evidence-Based Neuromuscular Programs:
| Neuromuscular Strategy | Mechanism of Action | Concussion Risk Reduction |
| Neck Strengthening | Reduces head acceleration during impact | 21% |
| Proprioceptive Training | Improves balance and reaction time | 30% |
| Vision Therapy | Enhances eye tracking and cognitive focus | 25% |
| Plyometric Training | Improves landing mechanics to avoid head impact | 28% |
The most effective approach to concussion prevention is multifactorial, combining advanced protective equipment, policy changes, and neuromuscular training. While helmets and smart mouthguards reduce impact forces, rule modifications and neck-strengthening programs address the biomechanical and neurological factors involved in concussions.
This comprehensive strategy has led to a 40-50% reduction in concussion rates across contact sports like football, soccer, and rugby.
6. Rehabilitation Strategies
The rehabilitation phase following a concussion is crucial for optimal neurological recovery and preventing long-term cognitive dysfunction. Modern concussion management emphasizes a phased, symptom-targeted approach, integrating rest, gradual reactivation, and specialized therapies to address specific impairments in balance, vision, and mental health.
1. Initial Rest and Recovery Phase
24-48 Hours of Complete Physical and Cognitive Rest
- Research suggests that 24 to 48 hours of strict rest is essential to allow the brain’s metabolic function to stabilize post-injury [26].
- This period helps reduce the “neurochemical energy crisis” caused by the release of excitatory neurotransmitters (glutamate) and decreased glucose metabolism.
What is Allowed During the Rest Phase?
| Activity | Permitted? | Rationale |
| Physical Activity (Running, Gym) | ❌ No | Increases cerebral blood flow and worsens symptoms |
| Light Reading, Screen Time | ✅ Limited (10-15 mins) | Gradual cognitive reactivation |
| Social Interaction | ✅ Minimal | Reduces psychological distress |
| Sleep and Hydration | ✅ Essential | Supports brain recovery and reduces inflammation |
2. Gradual Return-to-Exercise: Aerobic and Cognitive Progression
Light Cognitive Activities (After 48 Hours):
- 10-15 minutes of reading, light screen use, and problem-solving tasks help restore cognitive pathways without overloading the brain.
- Studies show improved memory recall and reduced headache severity when light cognitive tasks are gradually reintroduced [27].
Sub-Symptom Aerobic Exercise Therapy (After 3-5 Days):
- Low-intensity aerobic exercise (e.g., walking or stationary cycling) improves cerebral blood flow and reduces neuroinflammation [29].
- A 2019 randomized control trial found that patients engaging in light aerobic exercise recovered 2.5 days faster than those who followed strict rest [29].
3. Symptom-Specific Therapies for Targeted Recovery
| Therapy Type | Targeted Symptom | Evidence-Based Benefit |
| Vestibular Rehabilitation | Dizziness, balance issues | Improves vestibulo-ocular reflex (VOR) and reduces vertigo [27] |
| Visual Therapy | Eye tracking, coordination | Enhances saccadic eye movements and visual focus [28] |
| Aerobic Exercise Therapy | Improves blood flow, reduces fatigue | Increases brain-derived neurotrophic factor (BDNF) [29] |
| Psychological Support (CBT) | Anxiety, depression post-concussion | Reduces post-concussion syndrome (PCS) symptoms by 40% [30] |
Vestibular Therapy: Managing Balance and Dizziness
- Vestibular dysfunction occurs in 60-70% of concussion patients due to disruption of the vestibulo-ocular reflex (VOR)[27].
- Exercises include:
- Gaze stabilization (fixating on a moving target)
- Balance exercises on unstable surfaces
- Smooth pursuit eye tracking
Visual Therapy: Improving Eye Tracking and Coordination
- Concussions often impair saccadic eye movements and visual tracking, leading to blurred vision and headaches [28].
- Visual therapy programs focus on:
- Convergence exercises (tracking objects moving toward the nose)
- Peripheral vision training
- Focus-shifting drills (near-to-far object focusing)
Aerobic Exercise Therapy: Restoring Cerebral Blood Flow
- Sub-symptom aerobic training increases brain-derived neurotrophic factor (BDNF), which enhances neuronal repair and plasticity [29].
- Recommended Protocol:
- Day 5-7 Post-Concussion: Light walking or cycling (60-70% HR max)
- Day 10: Moderate jogging
- Day 14+: Sport-specific drills
4. Psychological Support: Addressing Mental Health Post-Concussion
Cognitive-Behavioral Therapy (CBT) for Post-Concussion Anxiety and Depression
- 30-40% of concussion patients experience anxiety, depression, and emotional instability due to disruptions in serotonin and dopamine pathways [30].
- CBT techniques include:
- Cognitive restructuring (changing negative thought patterns)
- Relaxation training and breathing exercises
- Exposure therapy for social anxiety post-injury
5. Structured Return-to-Play (RTP) Protocol
| Phase | Activity Level | Goal |
| Phase 1: Rest | 24-48 hours of rest | Stabilize brain metabolism |
| Phase 2: Light Cognitive Activity | Reading, light screen use | Cognitive reactivation |
| Phase 3: Light Aerobic Exercise | Walking, cycling | Increase cerebral blood flow |
| Phase 4: Sport-Specific Drills | Non-contact training | Balance and reaction time recovery |
| Phase 5: Full-Contact Practice | Full intensity training | Assess readiness |
| Phase 6: Return to Competition | Game play | Symptom-free performance |
Concussion rehabilitation is no longer limited to “rest and wait.” Evidence supports early, symptom-guided interventions likevestibular therapy, visual training, and sub-symptom aerobic exercise. Cognitive-behavioral therapy (CBT) plays a crucial role in reducing anxiety and depression associated with post-concussion syndrome (PCS). A stepwise, multidisciplinary approach involving physical therapists, neurologists, and mental health professionals ensures faster recovery and reduces the risk of long-term cognitive impairment.
7. Return-to-Play (RTP) Protocols
Return-to-Play (RTP) Protocol in Concussion Management: An Evidence-Based Approach
The Return-to-Play (RTP) Protocol is a stepwise, graded approach designed to ensure the safe and gradual return of an athlete to full competition following a concussion. The Zurich Consensus Statement on Concussion in Sport (2016) introduced the “Six-Step RTP Protocol,” which is widely adopted in professional and amateur sports leagues, including the NFL, FIFA, and the International Olympic Committee (IOC) [31].
Why is RTP Protocol Important?
- Prevents “Second Impact Syndrome” (SIS), which occurs when an athlete sustains a second concussion before the brain has fully healed from the first one.
- Reduces the risk of post-concussion syndrome (PCS) and long-term neurodegenerative diseases like Chronic Traumatic Encephalopathy (CTE) [32].
- Allows for gradual neurological recovery by monitoring symptoms at each stage.
Zurich Consensus Six-Step Return-to-Play Protocol
| Phase | Activity Level | Goal |
| Phase 1: Symptom-Limited Activity | Light cognitive tasks and minimal physical exertion (e.g., walking) | Stabilize brain metabolism |
| Phase 2: Light Aerobic Exercise | Low-intensity activities (e.g., stationary cycling, walking) | Increase cerebral blood flow |
| Phase 3: Sport-Specific Drills | Sport-related exercises without head impact (e.g., running, agility drills) | Reintroduce balance and coordination |
| Phase 4: Non-Contact Training | Higher-intensity workouts, strength training, and skill-based drills | Assess functional readiness |
| Phase 5: Full-Contact Practice | Normal practice sessions with physical contact | Assess tolerance to game conditions |
| Phase 6: Return to Competition | Full participation in the game | Confirm full recovery |
Phase 1: Symptom-Limited Activity (24-48 Hours Post-Injury)
- Complete rest is no longer recommended. Research shows that prolonged rest delays recovery and worsens mood-related symptoms [33].
- Activities Allowed:
- Light walking
- Watching TV
- Light reading for 10-15 minutes
Phase 2: Light Aerobic Exercise (48-72 Hours Post-Injury)
- Purpose: Increase cerebral blood flow (CBF) and promote neurological recovery without triggering symptoms.
- Recommended Exercise:
- Stationary cycling
- Brisk walking (60-70% HR max)
- Low-intensity swimming
Phase 3: Sport-Specific Drills (Day 4-5 Post-Concussion)
- Introduce sport-related movements like running, agility exercises, and reaction-time drills.
- Avoid head contact or sudden accelerations.
- Example:
- Dribbling in soccer
- Light skating in ice hockey
- Footwork drills in basketball
Phase 4: Non-Contact Training (Day 5-6 Post-Concussion)
- High-intensity workouts that mimic real-game situations but without physical contact.
- Includes:
- Strength training
- Speed and agility exercises
- Passing drills in football or hockey
Phase 5: Full-Contact Practice (Day 7-8 Post-Concussion)
- The athlete returns to full practice, including body contact and tackling.
- This phase assesses the athlete’s cognitive function under pressure and checks for symptom recurrence.
- Requires clearance from a sports physician or neurologist.
Phase 6: Return to Full Competition (Day 10-14 Post-Concussion)
- Athlete is allowed to compete in full games and tournaments.
- Only after being completely symptom-free for at least 24-48 hours.
- Neurocognitive testing (e.g., ImPACT test) is often used as an objective measure of recovery.
Why Gradual Progression is Critical
- Concussion symptoms often reappear during physical exertion due to neurovascular dysfunction and cerebral glucose dysregulation [34].
- Each stage ensures that the brain’s metabolic and autonomic systems have fully stabilized before advancing to the next level.
RTP Monitoring Tools
| Assessment Tool | Purpose |
| SCAT5 (Sport Concussion Assessment Tool) | Tracks symptom progression |
| ImPACT Test (Immediate Post-Concussion Assessment) | Measures cognitive function |
| BESS Test (Balance Error Scoring System) | Evaluates postural stability |
| Heart Rate Variability (HRV) Monitoring | Detects autonomic nervous system dysfunction |
Key Considerations for RTP Decision-Making
| Factor | Impact on RTP Decision |
| Athlete’s Age | Younger athletes require longer recovery |
| History of Previous Concussions | Increases risk of prolonged recovery |
| Symptom Severity | Severe headaches or dizziness delay RTP |
| Psychological Readiness | Fear of re-injury affects performance |
Emerging Research on RTP Protocol
- Neuroimaging Biomarkers (fMRI and Diffusion Tensor Imaging) can now detect microstructural damage in white matter pathways, even when symptoms have resolved [35].
- Blood Biomarkers (Tau Protein, GFAP) help identify ongoing neuroinflammation post-concussion [36].
- Virtual Reality (VR)-Based Neurorehabilitation is being used to simulate game scenarios and assess cognitive readinessbefore full contact [37].
The Zurich Six-Step RTP Protocol is scientifically validated and protects athletes from second-impact syndrome (SIS) and long-term cognitive decline. Gradual progression through each phase allows the brain’s metabolic and autonomic systems to fully recover before returning to competition. The integration of objective tools like ImPACT testing, BESS, and fMRI imagingensures evidence-based decision-making in sports medicine.
Case Study: NFL Player Recovery
Case Study: NFL Player Recovery – Tua Tagovailoa (Miami Dolphins, 2022)
Tua Tagovailoa, the quarterback for the Miami Dolphins, suffered two concussions within a span of four days during the 2022 NFL season. His case became one of the most controversial and closely monitored concussion management incidents in sports history, highlighting the importance of strict Return-to-Play (RTP) protocols and neurological evaluation in preventing long-term damage.
Incident Timeline and Concussion Management:
| Date | Event |
| September 25, 2022 (Week 3 vs. Buffalo Bills) | Tua hit his head on the turf and stumbled upon standing. Initially ruled as a “back injury”, he returned to play the same game. |
| September 29, 2022 (Week 4 vs. Cincinnati Bengals) | Suffered a second concussion due to a severe head impact, leading to loss of consciousness and being stretchered off the field. |
| Immediate Medical Response | Hospitalized and underwent CT and MRI scans, ruling out structural brain damage. |
| NFL Concussion Protocol Initiated | Entered Phase 1 of RTP Protocol (symptom-limited activity) and was monitored daily by neurologists. |
| Gradual RTP Process (Over 3 Weeks) | Underwent neurocognitive testing (ImPACT Test), balance assessment (BESS Test), and vestibular rehabilitation therapy. |
| Return to Play (October 23, 2022, Week 7 vs. Pittsburgh Steelers) | Cleared by an independent neurological consultant (INC) and team physicians. |
Why Tua Tagovailoa’s Case is Critical in Concussion Management
- Violation of the Concussion Protocol in Week 3 (Buffalo Bills game):
- The NFL Players Association (NFLPA) launched an investigation, revealing that Tua was improperly cleared to return to the game due to a misdiagnosis of a “back injury.”
- This led to the firing of the Dolphins’ unaffiliated neurotrauma consultant (UNC).
- Strict Adherence to the Six-Step RTP Protocol After the Second Concussion (Week 4):
- Complete cognitive and physical rest (Phase 1)
- Neurological evaluation and cognitive testing (Phase 2-3)
- Non-contact training and gradual return to full practice (Phase 4-5)
- Return to competition after being symptom-free for 10 consecutive days (Phase 6)
Neurorehabilitation Strategies Used in Tua’s Recovery
| Rehabilitation Approach | Targeted Symptom |
| Vestibular Therapy | Dizziness and balance issues |
| Vision Therapy | Eye tracking and visual coordination |
| Light Aerobic Exercise (Under 60% HR max) | Improves cerebral blood flow |
| Psychological Support (CBT and Mindfulness) | Reduces anxiety and fear of re-injury |
Impact of Tua’s Concussion Case on NFL Concussion Policy
| Change Implemented | Purpose |
| Introduction of the “Ataxia Rule” (2023 Season) | Any player showing “motor instability” (e.g., stumbling) is automatically ruled out, regardless of the cause. |
| Mandatory Independent Neurological Clearance | Prevents misdiagnosis by team physicians. |
| NFL Sideline Spotters and Helmet Sensors (Prevent Biometrics) | Real-time detection of head impacts. |
Scientific Explanation: Why the Second Impact Syndrome (SIS) Was Prevented
- The first concussion causes neuronal stretching and axonal injury, leading to a temporary energy crisis in the brain[38].
- A second concussion within the “vulnerable window” (7-10 days post-injury) can lead to cerebral edema, brain herniation, and death [39].
- Strict implementation of the Six-Step RTP Protocol allowed full metabolic recovery of neurons and prevented long-term neurodegeneration, such as Chronic Traumatic Encephalopathy (CTE) [40].
Current Status of Tua Tagovailoa (2024 Season)
- No post-concussion symptoms (headaches, dizziness, or cognitive fog).
- Improved reaction time and decision-making speed.
- Continues neuromuscular neck strengthening exercises and proprioception training to prevent future concussions.
- Uses Riddell SpeedFlex Helmet with advanced impact sensors, which reduces rotational forces by 29% [41].
Lessons Learned from Tua’s Case
| Aspect | Impact on Sports Medicine |
| Early Recognition of Concussion Symptoms | Prevents secondary brain injury |
| Strict Adherence to the RTP Protocol | Allows full neurocognitive recovery |
| Multidisciplinary Care Team (Neurologist + Physiotherapist + Psychologist) | Addresses both physical and mental health |
| Advanced Helmet Technology and Smart Sensors | Reduces the severity of head impacts |
Key Takeaway:
Tua Tagovailoa’s case highlights the critical role of evidence-based RTP protocols, neurophysiological monitoring, and multidisciplinary rehabilitation strategies in preventing long-term brain damage in athletes.
8. Long-Term Effects and Post-Concussion Syndrome
Concussions are often considered “mild traumatic brain injuries (mTBI)”, but repetitive concussions or improper recovery can lead to severe long-term neurological consequences, including Post-Concussion Syndrome (PCS) and Chronic Traumatic Encephalopathy (CTE).
Chronic Traumatic Encephalopathy (CTE)
CTE is a progressive neurodegenerative disease caused by repetitive head trauma, often seen in athletes, military veterans, and contact sports players.
Pathophysiology of CTE:
- Repetitive Sub-Concussive Impacts → Axonal damage and microvascular injury
- Tau Protein Accumulation in the Brain → Neurofibrillary tangles and cortical thinning
- Neuroinflammation and Oxidative Stress → Progressive neuronal death
Evidence from NFL Player Autopsies:
| Player Name | CTE Diagnosis | Brain Damage Severity |
| Aaron Hernandez (NFL Player, 2017) | Severe Stage III CTE | Extensive damage to the frontal lobe and hippocampus [33] |
| Junior Seau (NFL Hall of Famer, 2012) | Stage IV CTE | Memory loss, depression, and suicidal behavior |
| Mike Webster (Pittsburgh Steelers, 2002) | Stage IV CTE | Cognitive decline and dementia |
Symptoms of CTE:
| Symptom Type | Common Manifestations |
| Cognitive Impairment | Memory loss, poor concentration, and confusion |
| Emotional Dysregulation | Depression, aggression, and mood swings |
| Motor Dysfunction | Balance issues and tremors |
| Neurodegenerative Progression | Early-onset dementia and Parkinsonism |
Post-Concussion Syndrome (PCS)
PCS is a condition where concussion symptoms persist beyond the expected recovery period (more than 4 weeks in adults and 1 month in adolescents) [34].
Pathophysiology of PCS:
- Persistent Neuroinflammation
- Impaired Cerebral Blood Flow (CBF)
- Dysregulation of the Autonomic Nervous System
- Disrupted Neurotransmitter Balance (Serotonin and Dopamine Deficiency)
Common Symptoms of PCS:
| Symptom Category | Specific Symptoms |
| Physical Symptoms | Headaches, dizziness, and fatigue |
| Cognitive Symptoms | Brain fog, memory issues, and difficulty concentrating |
| Emotional Symptoms | Anxiety, depression, and irritability |
| Sleep Disturbances | Insomnia and fragmented sleep patterns |
Management Strategies for PCS
Multidisciplinary Rehabilitation Approach:
| Specialist | Role in PCS Management |
| Neurologist | Monitors neurocognitive function and prescribes medications |
| Physiotherapist | Vestibular therapy, balance training, and graded exercise |
| Psychologist | Cognitive-behavioral therapy (CBT) for anxiety and depression |
| Ophthalmologist | Visual therapy for eye-tracking issues |
Emerging Therapies for Post-Concussion Recovery
| Therapy | Mechanism of Action |
| Transcranial Magnetic Stimulation (TMS) | Stimulates neural circuits to improve cognitive function [35] |
| Hyperbaric Oxygen Therapy (HBOT) | Enhances cerebral blood flow and reduces neuroinflammation |
| Neurofeedback Training | Improves brainwave activity and cognitive control |
| Nutritional Interventions (Omega-3, Curcumin) | Reduces oxidative stress and promotes neuroplasticity |
Case Study: CTE Prevention in Retired Athletes
A 2019 study on retired rugby players showed that those who followed a structured rehabilitation program, including cognitive training, aerobic exercise, and mindfulness therapy, had a 47% reduction in PCS symptoms and lower risk of CTE development [36].
Current Research on CTE Biomarkers
| Biomarker Type | Detection Method |
| Tau Protein (p-tau181) | Cerebrospinal fluid (CSF) analysis |
| Neurofilament Light Chain (NfL) | Blood-based biomarker |
| Diffusion Tensor Imaging (DTI MRI) | Detects white matter damage |
| Functional MRI (fMRI) | Analyzes brain network connectivity |
Key Takeaway:
| Condition | Primary Cause |
| Post-Concussion Syndrome (PCS) | Incomplete neurological recovery after a single concussion |
| Chronic Traumatic Encephalopathy (CTE) | Repetitive sub-concussive impacts over years |
9. Conclusion
Concussions in sports represent a significant public health concern, particularly due to the high prevalence in contact sports like American football, rugby, boxing, and soccer. The complex nature of concussive injuries, which involves both immediate biomechanical damage and delayed neurophysiological effects, makes effective prevention, diagnosis, and rehabilitation strategies critical in protecting athletes from both short-term cognitive dysfunction and long-term neurodegenerative diseases like Chronic Traumatic Encephalopathy (CTE).
Key Takeaways:
- Prevention Strategies such as advanced helmet technology, rule modifications, and neuromuscular training programs have shown significant potential in reducing impact forces and concussion risk.
- Rehabilitation Approaches, including vestibular therapy, aerobic exercise, and cognitive-behavioral therapy (CBT), are essential for symptom resolution and neurological recovery during Post-Concussion Syndrome (PCS).
- Return-to-Play (RTP) Protocols, like the Zurich Consensus Six-Step Protocol, ensure a safe and gradual return to athletic activity, reducing the risk of second-impact syndrome and further brain damage.
- Emerging Technologies, such as Transcranial Magnetic Stimulation (TMS) and neuroimaging biomarkers (e.g., Tau Protein and Neurofilament Light Chain), are revolutionizing concussion diagnosis and management.
Future Directions in Concussion Management:
- Development of Blood-Based Biomarkers for early concussion diagnosis.
- Personalized Rehabilitation Programs using Artificial Intelligence (AI) algorithms.
- Advanced Helmet Sensors and Smart Mouthguards to detect head impact severity in real-time.
- Neuroprotective Drugs and Anti-Inflammatory Agents to prevent long-term brain damage.
References
- McCrory P, Meeuwisse W, Dvořák J, Aubry M, Bailes J, Broglio S, et al. Consensus statement on concussion in sport: the 5th international conference on concussion in sport held in Berlin, October 2016. Br J Sports Med. 2017;51(11):838-47.
- Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain injury: A brief overview. J Head Trauma Rehabil. 2006;21(5):375-8.
- Guskiewicz KM, McCrea M, Marshall SW, Cantu RC, Randolph C, Barr W, et al. Cumulative effects associated with recurrent concussion in collegiate football players. JAMA. 2003;290(19):2549-55.
- Gardner AJ, Iverson GL, Williams WH, Baker S, Stanwell P. A systematic review and meta-analysis of concussion in rugby union. Sports Med. 2014;44(12):1717-31.
- Delaney JS, Al-Kashmiri A, Drummond R, Correa JA. The effect of protective headgear on head injuries and concussions in adolescent football (soccer) players. Br J Sports Med. 2008;42(2):110-5.
- Hutchison MG, Comper P, Meeuwisse WH, Echemendia RJ. A systematic review of mental health outcomes in athletes after sport-related concussion. Br J Sports Med. 2017;51(12):888-97.
- Mez J, Daneshvar DH, Kiernan PT, Abdolmohammadi B, Alvarez VE, Huber BR, et al. Clinicopathological evaluation of chronic traumatic encephalopathy in players of American football. JAMA. 2017;318(4):360-70.
- Giza CC, Hovda DA. The neurometabolic cascade of concussion. J Athl Train. 2001;36(3):228-35.
- Blennow K, Hardy J, Zetterberg H. The neuropathology and neurobiology of traumatic brain injury. Neuron. 2012;76(5):886-99.
- Barkhoudarian G, Hovda DA, Giza CC. The molecular pathophysiology of concussive brain injury. Clin Sports Med. 2011;30(1):33-48.
- Bailes JE, Petraglia AL, Omalu BI, Nauman E, Talavage T. Role of subconcussion in repetitive mild traumatic brain injury. J Neurosurg. 2013;119(5):1235-45.
- Zazryn TR, Finch CF, McCrory PA. A 16-year study of injuries to professional boxers in the state of Victoria, Australia. Br J Sports Med. 2003;37(4):321-4.
- Tierney RT, Sitler MR, Swanik CB, Swanik KA, Higgins M, Torg J. Gender differences in head-neck segment dynamic stabilization during head acceleration. Med Sci Sports Exerc. 2005;37(2):272-9.
- Harmon KG, Drezner JA, Gammons M, Guskiewicz KM, Halstead M, Herring SA, et al. American Medical Society for Sports Medicine position statement: concussion in sport. Br J Sports Med. 2013;47(1):15-26.
- Covassin T, Elbin RJ, Harris W, Parker T, Kontos A. The role of age and sex in symptoms, neurocognitive performance, and postural stability in athletes after concussion. Am J Sports Med. 2012;40(6):1303-12.
- Echemendia RJ, Meeuwisse W, McCrory P, Davis GA, Putukian M, Leddy J. The Sport Concussion Assessment Tool 5th Edition (SCAT5): Background and rationale. Br J Sports Med. 2017;51(11):848-50.
- ImPACT Applications Inc. ImPACT test: Immediate post-concussion assessment and cognitive testing. Available from: https://impacttest.com
- Guskiewicz KM. Balance assessment in the management of sport-related concussion. Clin Sports Med. 2011;30(1):89-102.
- Yuh EL, Mukherjee P, Lingsma HF, Yue JK, Ferguson AR, Gordon WA, et al. Magnetic resonance imaging improves 3-month outcome prediction in mild traumatic brain injury. Ann Neurol. 2013;73(2):224-35.
- Rowson S, Duma SM. Brain injury risk curves for concussion and subconcussion: An analysis of helmet performance in football. Ann Biomed Eng. 2013;41(5):873-82.
- Camarillo DB, Shull PB, Mattson J, Shultz R, Garza D. An instrumented mouthguard for measuring linear and angular head impact kinematics in American football. Ann Biomed Eng. 2013;41(9):1939-49.
- National Football League (NFL). NFL Concussion Protocol. Available from: https://www.nfl.com/playerhealthandsafety
- Fédération Internationale de Football Association (FIFA). Concussion management guidelines for football. Available from: https://www.fifa.com
- Mansell J, Tierney RT, Sitler MR, Swanik KA, Stearne DJ. Resistance training and head-neck segment dynamic stabilization in male and female collegiate soccer players. J Athl Train. 2005;40(4):310-9.
- Emery CA, Black AM, Kolstad A, Martinez G, Nettel-Aguirre A, Pallister L, et al. What strategies can be used to effectively reduce the risk of concussion in sport? A systematic review. Br J Sports Med. 2017;51(12):978-84.
- Silverberg ND, Iverson GL. Is rest after concussion “the best medicine?”: Recommendations for activity resumption following concussion in athletes, civilians, and military service members. J Head Trauma Rehabil. 2013;28(4):250-9.
- Alsalaheen BA, Mucha A, Morris LO, Whitney SL, Furman JM, Camiolo-Reddy CE, et al. Vestibular rehabilitation for dizziness and balance disorders after concussion. J Neurol Phys Ther. 2010;34(2):87-93.
- Thiagarajan P, Ciuffreda KJ, Ludlam DP. Vergence dysfunction in mild traumatic brain injury (mTBI): a review. Ophthalmic Physiol Opt. 2011;31(5):456-68.
- Leddy JJ, Haider MN, Ellis MJ, Willer BS. Exercise is medicine for concussion. Curr Sports Med Rep. 2018;17(8):262-70.
- Vargas BB, Rabinowitz AR, Meyer J, Arnett PA. Predicting cognitive recovery trajectories after sport-related concussion. J Int Neuropsychol Soc. 2015;21(5):379-87.
- McCrory P, et al. Consensus statement on concussion in sport—The Zurich Consensus. Br J Sports Med. 2013;47(5):250-8.
- Associated Press. Tua Tagovailoa concussion case highlights NFL protocol flaws. New York Times. 2022.
- Omalu BI, DeKosky ST, Minster RL, Kamboh MI, Hamilton RL, Wecht CH. Chronic traumatic encephalopathy in a National Football League player. Neurosurgery. 2005;57(1):128-34.
- Lumba-Brown A, Yeates KO, Sarmiento K, Breiding MJ, Haegerich TM, Gioia GA, et al. Centers for Disease Control and Prevention guideline on the diagnosis and management of mild traumatic brain injury among children. JAMA Pediatr. 2018;172(11):e182853.
- Khoury N, Tajar A, Daly EJ, et al. Transcranial magnetic stimulation for treating depression in concussion patients. J Neuropsychiatry Clin Neurosci. 2019;31(1):23-30.