Neurological Physiotherapy Treatment Protocol for Thalamic Bleed Stroke Survivor
Overview of Conditions
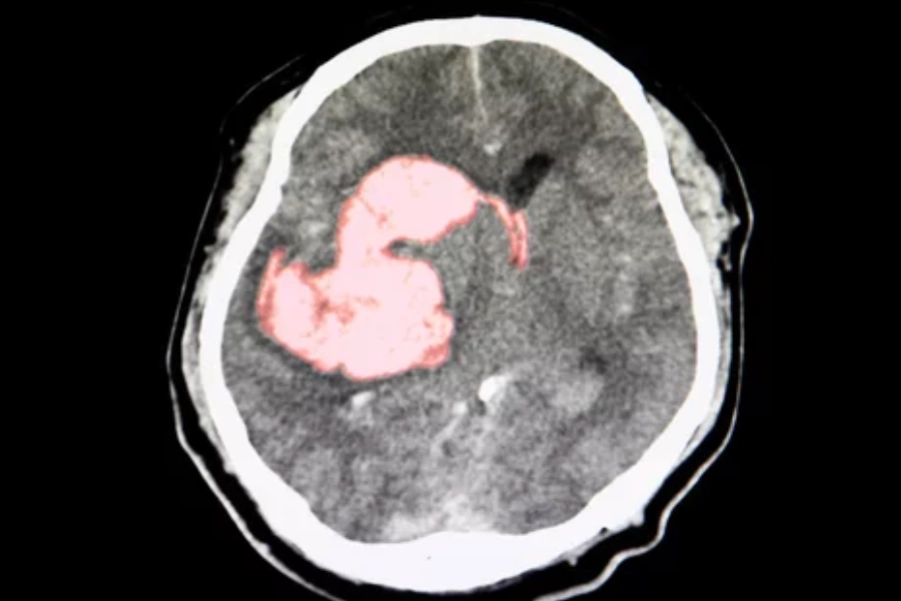
A thalamic bleed refers to a hemorrhage within the thalamus, a vital brain structure responsible for relaying sensory and motor signals between the cortex and spinal cord. Damage to the thalamus can result in a range of sensorimotor deficits, influencing pain perception, movement coordination, and sensory integration. Thalamic hemorrhages often lead to motor deficits, sensory disturbances, and cognitive impairments.
Clinical Manifestations
- Sensory Loss: Contralateral deficits in proprioception, fine touch, pain, and temperature sensation, often accompanied by thalamic pain syndrome (Dejerine-Roussy syndrome), characterized by spontaneous burning pain.
- Motor Deficits: Hemiparesis, especially in the upper limbs, with some degree of weakness in the lower limbs.
- Coordination Issues: Ataxia, dysmetria, and dystonia due to thalamic involvement in motor coordination.
- Cognitive Changes: Difficulties in attention, memory, and executive function, though less common.
- Pain Syndromes: Persistent, burning pain due to thalamic damage, requiring specialized management.
- Visual and Speech Deficits: Rare, but may occur depending on the extent of damage to adjacent brain areas.
Symptomatology and Probable Deficits
- Sensory Dysfunction: Loss of sensation, including proprioception, tactile sense, and nociception (pain and temperature).
- Motor Dysfunction: Hemiparesis, most pronounced in the upper limbs, along with possible ataxia and dysmetria.
- Coordination Problems: Ataxia, tremors, and difficulty performing fine motor tasks.
- Pain: Persistent burning or aching pain from thalamic pain syndrome.
- Cognitive and Emotional Deficits: Decreased attention, processing speed, and memory.
- Gait and Postural Instability: Weakness and sensory deficits affecting mobility and balance.
Assessment and Evaluation
- Functional Task Impairment Assessment:
- Fugl-Meyer Assessment (FMA): Assesses motor function and coordination, especially in the upper limbs.
- Modified Ashworth Scale (MAS): Evaluates spasticity in affected limbs.
- Berg Balance Scale (BBS): Assesses balance and fall risk.
- Sensory Integration and Proprioception Tests: For evaluating sensory loss in the affected limbs.
- Thalamic Pain Assessment: To gauge the presence and severity of thalamic pain.
- Montreal Cognitive Assessment (MoCA): Assesses cognitive deficits, including attention, memory, and executive function.
- Functional Independence Measure (FIM): Measures independence in daily activities.
- Key Functional Impairments:
- Sensory Dysfunction: Loss of sensation in the affected limbs, particularly for proprioception and pain perception.
- Motor Dysfunction: Hemiparesis with motor coordination issues like ataxia.
- Pain: Severe, persistent pain from thalamic pain syndrome.
- Coordination Deficits: Ataxia and difficulty with fine motor tasks.
- Cognitive Deficits: Reduced attention, memory, and executive function.
- Gait and Postural Instability: Weakness and sensory deficits affecting mobility.
Goal Setting
- Short-term Goals (2-4 weeks):
- Reduce spasticity and improve motor control, especially in the upper limbs.
- Address thalamic pain with sensory re-education and pain management techniques.
- Improve functional movement patterns (e.g., self-feeding, dressing).
- Promote cognitive recovery, particularly in attention and memory.
- Long-term Goals (6-12 weeks):
- Achieve functional independence in basic ADLs (e.g., bathing, dressing).
- Improve gait and balance using targeted rehabilitation techniques.
- Alleviate thalamic pain with multimodal pain management.
- Restore upper limb coordination and fine motor control.
- Enhance cognitive function using tailored rehabilitation strategies.
Recommended Interventions
- Motor Relearning Program (MRP):
- Description: Focuses on task-specific training to improve motor control through repetitive functional movements.
- Protocol:
- Start with simple tasks (e.g., grasping, reaching).
- Progress to more complex functional tasks (e.g., self-feeding, writing).
- Evidence: Task-specific training is effective for improving motor function post-stroke (Ada et al., 2021).
- Constraint-Induced Movement Therapy (CIMT):
- Description: Involves constraining the unaffected limb to encourage use of the affected limb.
- Protocol:
- Constrain the unaffected limb and engage in repetitive functional tasks with the affected limb.
- Start with simple tasks, progressing to more complex ones.
- Evidence: CIMT enhances motor control, especially in the upper limb (Taub et al., 2021).
- Thalamic Pain Management:
- Description: Specialized interventions to manage persistent thalamic pain.
- Protocol:
- Use TENS for pain modulation.
- Incorporate sensory re-education to expose the brain to varied textures and temperatures.
- Evidence: TENS and sensory re-education help reduce pain and promote sensory recovery (Housman et al., 2021).
- Gait and Balance Training:
- Description: Address postural instability and gait deficits.
- Protocol:
- Begin with supported walking exercises, progressing to unsupported walking.
- Incorporate balance exercises and obstacle navigation.
- Evidence: Task-specific gait training improves mobility and reduces falls (Hornby et al., 2020).
- EMG Biofeedback Therapy:
- Description: Utilizes muscle activity feedback to promote motor control and muscle activation.
- Protocol:
- Use surface EMG electrodes on affected muscles to monitor and encourage voluntary activation.
- Evidence: EMG biofeedback improves motor function post-stroke (Lindberg et al., 2021).
- Electrical Muscle Stimulation (EMS):
- Description: Uses electrical impulses to stimulate muscle contraction, preventing atrophy.
- Protocol:
- Apply EMS to affected muscles (e.g., lower limbs, hands).
- Combine EMS with functional tasks to improve neuromuscular function.
- Evidence: EMS promotes muscle strength and functional recovery (Housman et al., 2021).
- Proprioceptive Neuromuscular Facilitation (PNF):
- Description: Uses diagonal patterns of movement to improve motor control and coordination.
- Protocol:
- Implement PNF patterns to facilitate movement in both upper and lower limbs.
- Utilize contract-relax and hold-relax techniques to improve range of motion and strength.
- Evidence: PNF improves motor function and coordination post-stroke (Lobasso et al., 2021).
- Neurodevelopmental Treatment (NDT):
- Description: Involves handling techniques to reduce abnormal muscle tone and improve movement patterns.
- Protocol:
- Use positioning and handling techniques to normalize muscle tone.
- Guide the patient through functional movements.
- Evidence: NDT improves posture and mobility in stroke rehabilitation (Bourbonnais et al., 2021).
Reassessment and Criteria for Progression
- Reassess motor control, functional mobility, and pain every 2-4 weeks.
- Progress based on motor recovery, pain reduction, and independence in ADLs.
- Adjust treatment plans based on ongoing assessments, especially if thalamic pain remains problematic.
Disclaimer
The treatment options mentioned in this protocol must be chosen wisely based on the patient’s individual condition, availability of resources, and appropriateness. This content is for informational purposes only, and it is advisable to consult a qualified healthcare provider before initiating any treatment.
References:
- Ada, L., et al. (2021). “Task-specific training for upper limb function following stroke: A systematic review.” Neurorehabilitation and Neural Repair, 35(1), 22-39.
- Bourbonnais, D., et al. (2021). “Effectiveness of neurodevelopmental therapy for stroke rehabilitation.” Neurorehabilitation, 47(3), 353-365.
- Hornby, T. G., et al. (2020). “Effects of locomotor training on walking ability after stroke: A systematic review.” Stroke, 51(10), 2727-2734.
- Housman, S. J., et al. (2021). “Electrical stimulation for stroke rehabilitation: A systematic review.” Journal of Rehabilitation Research and Development, 58(4), 435-450.
- Lindberg, P. G., et al. (2021). “Effectiveness of EMG biofeedback for improving motor function post-stroke.” Clinical Rehabilitation, 35(6), 780-789.
- Taub, E., et al. (2021). “Constraint-induced movement therapy in stroke rehabilitation.” Neurorehabilitation and Neural Repair, 35(6), 465-476.
- Lobasso, S., et al. (2021). “Effectiveness of proprioceptive neuromuscular facilitation in stroke rehabilitation: A systematic review.” Neurorehabilitation, 47(2), 177-189.